A 10mm herniated disc is a fairly large disc herniation, although it is not the largest possible. It can cause severe pain in the lower back and legs as the disc presses on nearby nerves. The size of a herniated disc is important to consider when determining your treatment options.
Surgery may be necessary if the herniation is causing significant pain or other neurological symptoms, and larger herniations may be more likely to require surgery than smaller ones. Other treatments such as physical therapy, medications, steroid injections, and lifestyle changes may also help relieve the symptoms of a 10mm herniated disc. It’s important to work with your doctor to determine which treatments are right for you so that you can start feeling better soon.
Is a 5mm Disc Herniation Large?
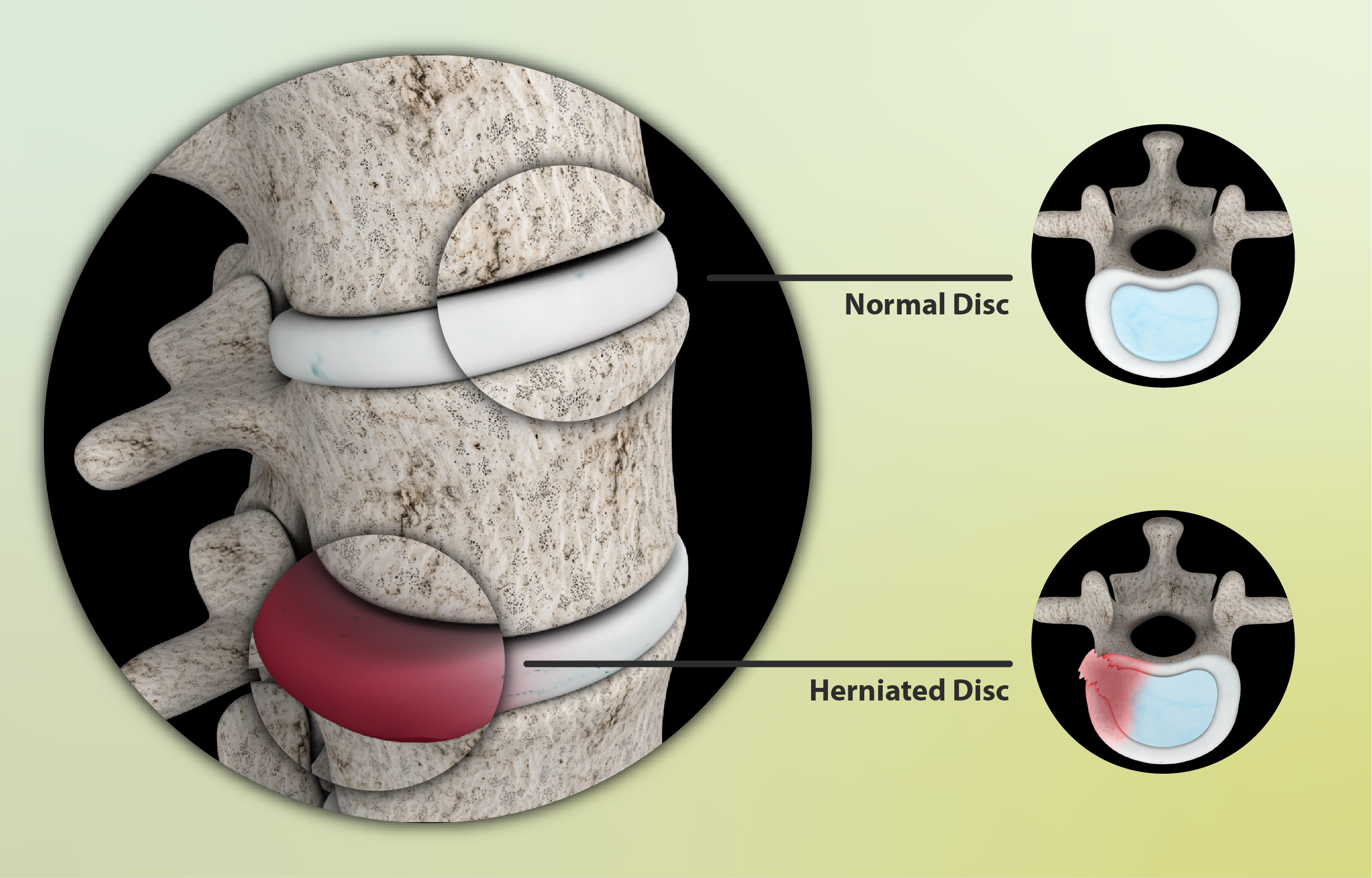
A disc herniation is a medical condition that occurs when the cushioning between the spinal vertebrae becomes damaged, resulting in the displacement of the cartilaginous material. The severity of a disc herniation can vary greatly depending on its size; a 5mm disc herniation is considered to be relatively mild compared to larger herniations.
While it can still cause pain and other symptoms such as tingling and numbness in certain areas of the body, these effects are typically much less severe than those caused by larger herniations. Therefore, while 5mm disc herniations may not be considered large, they should still be taken seriously and treated accordingly.
In general, if you experience any signs or symptoms associated with a disc herniation, it is important to seek medical attention in order to ensure that your injury does not worsen over time.
How Many mm Is Considered A Large Disc Herniation?
A large disc herniation is generally considered to be a herniation that is greater than 3 mm. This size of herniation can cause significant symptoms, including radiating pain, numbness, and weakness in the affected area. It may also cause difficulty with certain movements or activities such as bending or lifting heavy objects.
A large disc herniation can be extremely painful and disabling for those affected by it. Depending on the severity of the herniation, treatments may include physical therapy, medications, injections, or surgery. If left untreated it can lead to further complications such as nerve damage or paralysis. It is important to seek medical attention right away if you think you have a large disc herniation so that appropriate treatment can be given.
What Is The Most Common Disc Herniation Level?
The most common disc herniation level is the lumbar spine, or lower back. This is due to the fact that this area of the body carries a lot of weight and is responsible for supporting the majority of our movements. The discs between each vertebrae in this area can become damaged or herniated due to age, overuse, trauma, or degeneration.
Symptoms of a herniated disc at this level may include pain, numbness, tingling sensations, and muscle weakness. Treatment options such as physical therapy, rest, medications, injections, and surgery are available to help manage symptoms and treat the underlying cause. It’s important to seek medical attention if you suspect you may have a herniated disc at the lumbar spine level so that your doctor can properly diagnose and treat your condition.
How Many mm Is A Spinal Disc?
The spine is made up of 33 individual vertebrae, each separated by a thick cushioning disc. The discs are made up of an outer layer called the annulus fibrosus and an inner layer known as the nucleus pulposus. Each spinal disc has a height of between 4-6mm, depending on the region of the spine it is located in.
The discs act as shock absorbers for our body, allowing us to move without putting too much pressure on our vertebrae. They also provide flexibility to our spine and allow us to bend forward and backward. The thickness of these discs also helps protect the nerves that exit from the spinal cord.
Without these vital discs, we would be unable to move freely and would be at risk for significant injury due to increased friction between our vertebrae. It is important to maintain good posture and keep our discs healthy so that they can continue to provide support and cushioning for us throughout our lives.
How Many mm Is A Severe Disc Herniation?
A severe disc herniation is typically measured in millimeters (mm). It is difficult to give a precise measurement for a severe disc herniation as it can range from anywhere between 5-25mm. Generally speaking, a disc herniation of more than 5mm is considered to be large, and anything above 10mm is considered to be severe. A herniation over 20mm can be very severe and may require immediate medical attention.
The severity of the herniation often depends on where it occurs in the spine, as well as how much pressure or trauma has been applied to the affected area. If the herniation occurs in an area of the spine that contains nerves, such as the neck or lower back, then it may produce more serious symptoms than if it were located elsewhere.
Additionally, if there are any other signs of damage to the surrounding tissue or vertebrae, then this could affect how severe the herniation ultimately is.
How Many mm Is A Disc Herniation?
A disc herniation is typically measured in millimeters, usually ranging from 4mm to 6mm. Depending on the severity of the herniation and the area of the spine that has been affected, a disc herniation can range from 3mm to 10mm or even more.
For example, a herniation in an area of the neck may be larger than one in an area of the lower back due to greater movement and stress occurring in that particular region. The size of a disc herniation is also determined by its type; for instance, a bulging disc will be smaller than a protruding disc, which is when the inner material pushes out further past the surrounding tissue.
Ultimately, it’s important for your healthcare provider to accurately measure your herniated discs in order to develop an effective treatment plan.
What Is Considered A Massive Disc Herniation?
A massive disc herniation is a severe condition in which the nucleus pulposus, or the inner part of a spinal disc, has ruptured and bulges out of its normal position. This can occur in any part of the spine and can be extremely painful, as it puts pressure on nerves that cause pain to radiate through the body.
The most common type of massive disc herniation occurs in the lumbar region of the spine, where it is typically caused by extended periods of time spent sitting or standing, or being involved in high-impact activities like sports. In some cases, surgery may be necessary to restore full function to the affected area.
However, physical therapy and lifestyle modifications can often improve symptoms without the need for major interventions.
Does Size Of Disc Herniation Matter?
Size of disc herniation does matter when it comes to diagnosing a patient with this condition. It is important to understand the size of the herniation, as larger herniations can cause more pressure on the peripheral nerves and lead to greater pain and discomfort.
Smaller herniations may not be as painful, but they can still cause issues if left untreated. The size of the herniation can also help determine how best to treat it, as some treatments may work better for smaller or larger herniations than others. It is important to consult a doctor or specialist who can accurately assess the size of a disc herniation in order to determine the most effective course of treatment.
What are the 4 categories of disc herniation?
Disc herniation is a condition that affects the discs between the vertebrae of the spine. It occurs when the inner core of the disc pushes through its outer layer and puts pressure on the spinal nerves. There are four categories of disc herniation: Central, Paracentral, Foraminal, and Extraforaminal.
Central herniation is when the nucleus pulposus pushes into the central canal of the spinal cord, causing compression on nerve roots below and above it. Paracentral herniation is when there is an outward bulge in one direction or another but does not involve any contact with either side of the central canal.
Foraminal herniation occurs when a disc bulges enough to press against a nerve root as it exits from its foramen. Extraforaminal herniation happens when a disc bulges outside of its foramen and compresses a nerve root exiting from it. Each type of disc herniation can cause different symptoms depending on where it is located and how much pressure it puts on nearby nerves. Treatment may include pain medications, physical therapy, or even surgery in some cases.
Can a Disc Herniation Heal Itself?
Yes, a disc herniation can heal itself with proper rest and adequate physical therapy. It typically takes anywhere from several weeks up to several months for a disc herniation to heal on its own. It is important to note that some herniated discs may not heal themselves, and in those cases, surgery may be required.
To help the healing process, individuals should rest, avoid activities that increase pain or discomfort, and perform specific stretching and strengthening exercises. Additionally, over-the-counter medications such as ibuprofen can be taken to alleviate any pain associated with the condition. With proper care, many people are often able to return back to their normal activities without any issues.
Can an X-Ray Show a Herniated Disc?
Yes, an X-Ray can show a herniated disc. X-Rays use electromagnetic radiation to create an image of the inside of the body and can detect abnormalities in the spine, such as a herniated disc. The X-Ray will show the shape and position of the vertebrae, which can help diagnose a herniated disc.
It can also be used to measure the size of the disc and its alignment with adjacent vertebrae. An X-Ray cannot however show the extent of the nerve damage caused by a herniated disc or other serious conditions like a tumor or infection. For this reason, additional imaging tests may be required for further diagnosis and treatment planning.
Do Disc Herniations Shrink?
Do disc herniations shrink? Yes, they can. Disc herniations occur when the soft inner core of a spinal disc pushes through a weakened area of the outer wall of the disc, causing pain and other symptoms.
With rest, physical therapy and other treatments, the herniation may shrink or resolve on its own. In some cases, it is possible to reduce inflammation and pressure on the nerve with medications or physical therapy. Surgery may also be an option if conservative treatments fail to provide relief from pain and other symptoms. Ultimately, disc herniations may shrink over time depending on the severity of the injury and any other associated conditions.
Does Size Of Disc Herniation Matter?
The size of a disc herniation does matter when it comes to determining the severity of the injury. A small herniation may cause mild to moderate pain, while a large herniation can cause more serious symptoms such as numbness and tingling in the arms or legs. In some cases, a large herniation may result in nerve damage that can lead to paralysis or even death.
It is important to get an accurate diagnosis from a medical professional so that appropriate treatment can be administered. Surgery may be required for larger disc herniations depending on their location and the severity of symptoms. Physical therapy, stretching exercises and lifestyle modifications are often recommended as well for smaller disc herniations.